Dr. Ilan Gielchinsky
Robotic Surgeon
Minimally Invasive Cancer Surgeon
Consultant Urological Surgeon

®
Transperineal, MRI Fusion, Template Mapping Prostate Biopsy


Short Film (Hebrew)
This page contains information on prostate biopsy and diagnosis. Please feel free to contact me for any further questions.
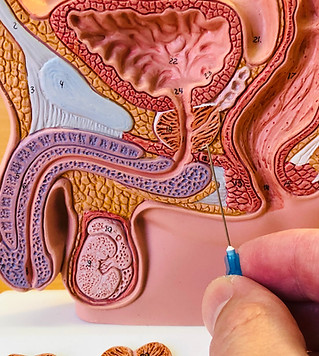
What is the Prostate?
The Prostate gland sits just under the urinary bladder and above the pelvic floor. The urine flows from the bladder through the prostate to the penis and outside (The Urethra). The Prostate produces seminal fluid (sperm cells are produced in the testicles). One of the proteins that the Prostate produces is called "PSA" (Prostate Specific Antigen) which is responsible for liquefaction of the seminal fluid.
What is Prostate Cancer?
Prostate Cancer is the most common cancer in men, and might effect 1 in 6. In most cases the cancer will be asymptomatic and will not effect the patients life (we call it insignificant prostate cancer). Nevertheless in some cases the cancer grade will be high, and as such, will require treatment.
What are the symptoms of Prostate Cancer?
Once ("Pre-PSA era"), Prostate cancer was sometimes diagnosed when patient was experiencing bone pain, urinary obstruction or blood in the urine. Since the 1990's, many patients are diagnosed with Prostate Cancer while asymptomatic.
How do we diagnose Prostate Cancer?
Diagnosis of Prostate Cancer is being done with a needle biopsy. We suspect Prostate Cancer when we have an abnormal PSA test, digital rectal examination or MRI imaging.
My GP says my PSA blood test is abnormal. What should I do?
PSA or in its full name "Prostate Specific Antigen" blood test, measures the level of this protein which is produced by the Prostate. The PSA itself is not a disease and its level might be elevated in cases such as Benign Prostate Hyperplasia (BPH or "enlarged prostate"), urinary tract infection, prostatitis and also in Prostate Cancer. The only thing you should do in case of abnormal PSA level is to come to the clinic for check-up and further evaluation.
What if during the meeting further evaluation is needed?
If during the meeting at the clinic, further investigation is needed, I will refer you to a mpMRI scan. This scan has no radiation, is not invasive (we do not need a rectal coil in the new machines) and is not painful. After the scan we will meet again and discuss further steps. Please bring the actual disc with you.
Why do you refer to mpMRI scan prior to biopsy?
mpMRI has over 93% sensitivity to significant prostate cancer lesions. In case of a suspicious area I can use the MRI scan in order to navigate and sample the lesion. In case that the MRI is intact we will evaluate if biopsy is needed. In most organs we use imaging prior to biopsy. For example, we use mammography prior to breast biopsy, or, we use CT scan prior to kidney biopsy. In the same manner we can use mpMRI prior to prostate biopsy.
How do you preform the biopsy?
The biopsy is being done as a day surgery procedure and taken in the operating theatre (OT). you arrive to the department and taken to the OT. We then put you to sleep for 15-30 minutes while taking the biopsy. After you wake up you are taken back to the department, drinking a cup of coffee and after urinating you can go home.
What is the difference between this biopsy and standard one?
The standard biopsy is being done at the clinic through the rectum, and is blind. 12 cores are being taken from 6 fixed parts of the back of the prostate under ultrasound. This biopsy has a few disadvantages. First, due to the rectal approach there are parts of the prostate that can not be sampled (Such as the anterior prostate). Next, the chances of infection that will need hospitalisation (sepsis) is 1:200. Finally, many patients describe it as a painful and unpleasant procedure. In transperineal, MRI fused, Template Mapping Biopsy we do not insert the needle through the rectum but through the Perineum (the skin behind the scrotum). By doing so we reduce the risk for infection to 1:2000. The needle can cover all areas of the prostate and we can sample 14-18 areas of the prostate, or every 5 mm. We start by navigating to the suspicious areas we found on your mpMRI scan (Biojet fusion system), and then we continue to take full mapping template. By doing so we increase the chances of diagnosing clinically significant prostate cancer by up to 30%. The anaesthesia prevents pain and reduces discomfort during the procedure. Another advantage of full mapping, on top of the higher detection rate, is that in case that future treatment is needed, we can evaluate if we can use focal therapy technique or how to refine our robotic surgery (By knowing where we need to be more radical to remove all cancer, or, be more liberal in order to spare the erection nerves, the bladder neck or sphincter).
What training did you do in order to perform this procedure?
After being fully trained as a Consultant Urological Surgeon in Hadassah Hebrew University Medical Centre, I have completed full fellowship in Robotic and Minimal invasive cancer surgery in St. Vincent's Hospital and the Garvan Institute of Medical Research, Sydney, Australia, under the supervision of Prof. Phillip Stricker who is one of the confounding father of this technique world-wide.
On Rectal biopsy (left) the needle crosses the rectum to reach the back of the prostate, thus have higher rate of infection (1:200) and limited range. On Transperineal Biopsy (Right), the needle crosses the skin, thus have extremely lower rate of infection (1:2000) and full range to all areas of prostate.


The MRI hologram we use during biopsy. The prostate in green and suspicious areas in red and blue.

The image on the left shows the prostate (Green) and anterior tumour (red) on MRI scan during biopsy. This area is unreachable with standard biopsy

The image on the left shows the prostate (green) and small tumour (red) on MRI scan. This allows me to navigate the needle directly to it.

